This article discusses what to do about suicidal ideation and being suicidal; however, we are coaches, not licensed clinicians. If you or someone you know is contemplating suicide or needs help, please call the National Suicide Prevention Lifeline at 988 or skip to the resources below now.
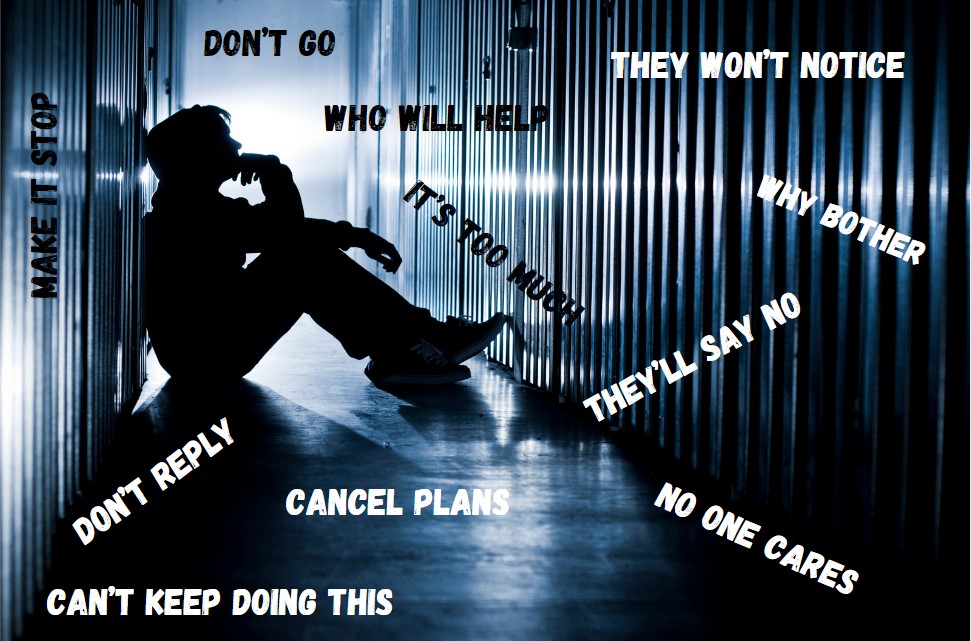
Cover Image: Original image from aurumarcus on iStock. Words added by author.
National Suicide Awareness Month
September has been National Suicide Awareness Month since 2008. First Responder Coaching has discussed this before – in fact, many times – and we’re not slowing down until the stats are null. We’re aware, you may say, now what?
With suicide remaining the number one cause of death among first responders, we’re still facing an uphill battle. Becoming a first responder seems to have more personal and mental risks than expected. Of course, suicide affects more than first responders, though first responders make up 1% of known suicide cases, so be advised that these resources are for almost all in need, and not one resource would turn away anyone in crisis.
Recognizing Suicidal Ideation in Others
First things first. How do you recognize suicidal ideation or thoughts/tendencies in others?
People are often afraid to jump to conclusions, offend, or invade a friend or coworker’s privacy. Maybe you feel it’s not your place to ask or judge.
But what would the other end look like if your instincts were correct and you did nothing?
Doesn’t feel comfortable either way, but suicide isn’t comfortable; it’s devastating.
When in doubt, please feel free to reach out to either FRC or one of the resources below and ask, even if it’s not about you. We have experienced folks here who can help you navigate your concerns and your conversation is confidential.
Signs in Others
This short list offers some warning signs of suicidal ideation, but be aware that a person truly suicidal (not just thinking but planning) will be a good actor and do their best to hide it.
- Withdrawal – A person contemplating or planning suicide will begin to withdraw from friends, family, and coworkers. They will not discuss their burdens and may dismiss any concerns you have.
- Communication – Conversations will be short, even curt, and feel unwelcome. Answers may be dismissive and calls may turn to short texts.
- Behavior – Activities this person once participated in and enjoyed will no longer excite them and they will often decline invitations. All enjoyment may seem unimportant to them.
- Anger or Offense – They may try to cut you off or turn you away so cutting ties is easier. They may even offend you or seem angry to make you not want to help.
What To Do
Not every tactic works for every person in every situation, but here are some ideas we’ve talked about before that can help.
- Be blunt and ask, “Are you going to hurt yourself? Are you safe?” If they are, they will stumble or they look left before answering. They’re trying to find a way to lie or they will be quiet about it since they don’t want attention.
- Don’t get upset. Remain patient and open. Let them know you’re willing to bear their emotions by showing patience and calmness.
- Body language is vital. Be smaller. If they’re standing, sit down. Don’t cross your arms or seem inconvenienced. Suicide is all about guilt and shame so don’t perpetuate that.
- Be genuine and supportive. Be fully vested in wanting to help or it could make things worse. They’ve already felt let down and are even more vulnerable now.
- Don’t shy away from helping out of a false sense of respect. Just because they’re first responders doesn’t mean they can’t be sectioned like everyone else. They deserve and need the same care as everyone else. Treat them like all other people in need of care.
- Realize you can’t save everyone. That’s a hard pill to swallow but it needs to be said. Do what you can and reach out, but ultimately you cannot control the actions of others. Do what you can and don’t be shy to get your own support.
- Call a resource listed below for more specific help for the person you care about.
Recognizing Suicidal Ideation in Yourself
We put on the tough exterior, the I’m-fine face, acting like the trauma we bear and the trauma we see is just another day at work. It is, but it isn’t.
Look, it’s okay to be stressed and have one of those days (or weeks), but we urge you to pay attention to yourself. If you’re feeling or thinking or doing any of the below warning signs, please talk to someone. No one has to know; just do it for the people you love.
Signs in Yourself
It’s self-check time. Ask yourself if any of the below seems close to the mark for you. If even a possible yes is on the horizon, please reach out. You could be saving yourself from a dangerous road. At worst, you spend a little time talking about you. At best, you realize you need help and to change direction in life. You may even save a life you never considered saving before: your own. Seriously, take time for you here and learn to recognize suicidal ideation.
- Withdrawal – Are you slipping away from people you once talked to more? Are you talking less and shortening your answers? Are you opting for texts or emails more than usual? Are you avoiding people more than you used to? Are you trying to become invisible? Are you removing attachments?
- Dark Mindset – Are you perpetuating a thought process where you don’t matter or you’re not wanted? Are you overall more negative than typical for you? Are you imagining scenarios of people with you out of the picture?
- Behavior change – Are you acting differently? Aside from the above, are you less interested in things that you once enjoyed? Do you find it harder and harder to feel good about anything? Are you more easily annoyed or angry?
What To Do
The most important thing to do is to reach out. There’s no need to bear suicidal ideation alone. Many support you and there are many channels to find that support now. Here are somethings you can do right now.
- Have a foundation now, not later. You need to gather a village of support. It’s much harder to build it once things get ugly so don’t wait to build it. That said, it’s also never too late. Parts of that plan include:
- I will listen when someone tells me I’m not acting myself or I’m acting differently somehow.
- I will be honest with those who are concerned about me.
- I will self-check and check in when things get tough or dark.
- I have a list of people or places to call for help when needed.
- Self-check, especially if you have depression or PTSD. Self-checking is important for everyone.
- What’s causing me to feel this way? Anger is a secondary emotion often from fear or sadness.
- Be self-aware. What are your normal limits? Are you usually happy, quiet, etc. Are you outside of your norm?
- Are you distancing or changing your behavior? Are you stopping or doing less of the things you enjoy? Are you talking to certain people less? If so, why?
- Ground yourself.
- Use grounding techniques.
- Meditation isn’t that hokey. Seriously, try it.
- Do something you enjoy. Go for a hike, to the gym, or for a bike ride. Move. Breathe. Feel alive.
- Reach out! See below for resources or talk to someone you know for help.
- Just like having ICE (In Case of Emergency) in our phones, we need a list of resources, a village of support, to pull from in an emergency. If you’re feeling this way, it’s an emergency. You don’t deserve to feel this way. Let’s get you to a better place.
More Resources
Please consider the first three in a true emergency, but we hope it doesn’t come to that. Always think ahead for the best possible outcome, but know your channels should things go sideways.
- 988 Suicide & Crisis Lifeline: Formerly the National Suicide Prevention Lifeline, you can also chat or text.
- Local PD business line: For those trying to help in an emergency from out of state, call the business line to the local police station. Check the website for multiple numbers as some may have limited hours but there will be a 24-hour line. Be sure you know the person’s address and any other pertinent information you need to relay.
- 911: This is always an option in any emergency as well if needed.
- Addiction Center: While not first responder specific, Addiction Center is owned by Recovery Worldwide, a national informational marketing umbrella for several addiction recovery-related properties. Addiction Center works with nationally recognized treatment facilities to provide treatment counseling, rehab placement and insurance/financial consultations for those seeking help.
- Peer support systems: These are in place for many departments and unions so be sure you have that information. Don’t wait for a crisis. Have their number now! For a good starting list, click here for SAMHSA’s list. Here are some we like too:
- First Responder Support Network
- First Responders Foundation
- Peer Connect by First Response
- Responder Life
- Stay Fit for Duty
- Peer Support Foundation
- Responder Strong
- First Responder Project – Crisis lines for first responders here too!
- First Responder Coaching – We’re composed of and service all first responders and families. We listen. We know you. We understand.
Don’t Wait
You wouldn’t want to wait for a house fire to be fully involved before calling the fire department. So, don’t wait on mental health either. Know the warning signs and have a prevention system in place.
Don’t think you have a support system? Think again. We’ve been doing peer support for years now and there’s a network of first responders spanning the globe. Yes, globe.
Think you can’t reach out because it’s not about you or you’re not a first responder? Wrong. You can and, if needed, you will directed to the help you (or your loved one) need(s).
Check out the resources and please help lower those stats. Suicidal ideation is no passing fad. We need to get ahead of this mental health crisis, today.